INVITED COMMENTARIES ON A GRAPH: Proportion of post-term births in European countries
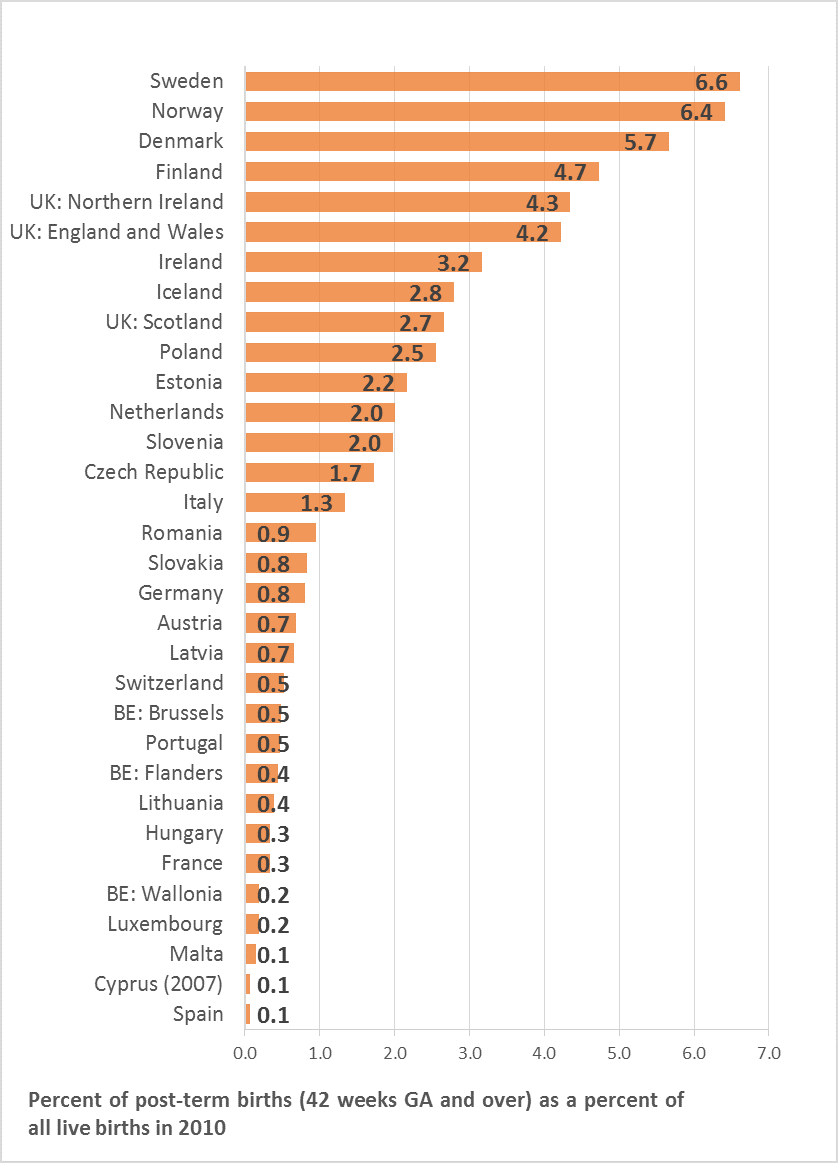 Data from the European Perinatal Health Report 2010. The Health and care of women and babies in Europe in 2010
Data from the European Perinatal Health Report 2010. The Health and care of women and babies in Europe in 2010
A perspective from Sweden:
"The Swedish figures reflects the obstetric guidelines that are used in most Swedish counties: If no obstetric complications are present, no interventions are carried out until the pregnancies have reached 42 completed weeks. Recently, these guidelines have been questioned and they are under revision in many counties. A national, randomized trial is soon to be commenced, which is scheduled to last two years [i]. Most counties are waiting for the results from this trial before they reconsider the current obstetric guidelines regarding prolonged pregnancies."
-Dr. Karin Källen
Dr. Karin Källen, Professor in the Department of Obstetrics and Gynaecology at Lund University, and Methodological Support Unit, National Board of Health and Welfare, Sweden
Post-term variation in Europe:
"Maybe we are trapped by the words. A “preterm” or “post-term” birth sounds less desirable and satisfactory than a term birth. As defined by ICD-9 and 10, a term birth is between 37+0 and 41+6, suggesting that, anything outside that range is abnormal[ii]. In addition, the Cochrane systematic review gives strong evidence: routine induction at 41 weeks reduces the incidence of stillbirth[iii].
Certainly, the PERISTAT data must reflect this, and countries with the highest prevalence of births at ≥42 weeks must have the highest rates of stillbirths?
Contrary to expectations, however, the four countries with the highest prevalence of births at ≥42 weeks are Nordic countries, and their stillbirth rates are among the lowest in Europe as are their rates of induction and caesarean section (CS). In the figure describing the proportion of post-term births, the Nordic countries are followed by UK and Ireland, who are not as successful as the Nordic countries for stillbirth and CS rates, but have results which are in line with the Western European average.
Once more, it is impossible from these observational data to do anything else than generate further questions.
Some questions are purely clinical:
- Would the stillbirth rate be lower in the Nordic countries if they did more inductions at 41 weeks? A randomised trial in Sweden should provide some answers to this question (see comment from Dr. Källen).
- What surveillance is done in the Nordic countries, in the UK and Ireland, for women who are beyond their due date? And if there is such surveillance, when does it start?
- Do Nordic, British and Irish women participate in decisions regarding induction or waiting after 41 weeks, and what type of information concerning advantages and drawbacks is provided?
Some other questions are conceptual, or quasi philosophical:
- Is the evidence from the randomised trials, that induction at 41+ weeks decreases the risk of stillbirth without increasing CSs reproducible? Unselected induction of labour is associated with an increases of CS rate in many circumstances. Information in the randomised trials is insufficient regarding both the Bishop score and exact gestational age of women who participated. The likelihood of a successful induction differs substantially between a mature cervix at 41+6 weeks and an immature cervix at 41+0 weeks.
- Is it (just) possible that Nordic women have a longer median length of gestation? Some have suggested ethnic differences in gestational length[iv].
- Is it not tautological to wonder whether stillbirth does not increase as pregnancy duration increases? Implicitly it must. The question may well be about numbers needed of inductions to avoid one stillbirth or to bring on one caesarean? A useful example of a very similar question can be found in the RCOG green top guideline where it is shown that vaginal birth after CS (VBAC) will increase the risk of hypoxic ischaemic encephalopathy from 0,01% to 0,08% while it decreases the risk of maternal death from 0,013% to 0,004% and significantly decreases the risk of abnormally adherent placenta in a next pregnancy[v]. With such information, families assisted by maternity carers can make a balanced choice.
In summary, it would probably be unwise for countries who are routinely offering induction at 41 weeks to change their practice tomorrow. However, this is part of the more general discussion on when should interventions become routine, do babies and mothers benefit, and why do we want babies to be like calibrated apples."
-Dr. Sophie Alexander
Dr. Sophie Alexander is an obstetrician and professor in the Perinatal Epidemiology and Reproductive Health Unit at Université Libre de Bruxelles, and Euro-Peristat Scientific Committee member from Belgium
References
[i] Elden H, Hagberg H, Wessberg A, Sengpiel V, Herbst A, Bullarbo M, Bergh C, Bolin K, Malbasic S, Saltvedt S, Stephansson O, Wikström AK, Ladfors L, Wennerholm UB. Study protocol of SWEPIS a Swedish multicentre register based randomised controlled trial to compare induction of labour at 41 completed gestational weeks versus expectant management and induction at 42 completed gestational weeks. BMC Pregnancy Childbirth. 2016 Mar 7;16:49. doi: 10.1186/s12884-016-0836-9. RCT registration: Current Controlled Trials, ISRCTN26113652
[ii] Ninth revision of the International Classification of diseases Manual of the international statistical classification of diseases, injuries, and causes of death, Volume 1. Geneva, World Health Organization, 1977.
[iii] Gülmezoglu AM, Crowther CA, Middleton P, Heatley E. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database of Systematic Reviews 2012, Issue 6. Art. No.: CD004945. DOI: 10.1002/14651858.CD004945.pub3
[iv] Papiernik E, Alexander GR, Paneth N. Racial differences in pregnancy duration and its implications for perinatal care. Med Hypotheses. 1990 Nov;33(3):181-6
[v] RCOG Green top guideline 45 Birth after previous caesarean section, 2014 https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_45.pdf last accessed 11 June 2017

